NICU Life
10% of babies born in the U.S. wind up in the NICU for one reason or another. Often times, it is expected and planned for, especially if the baby is growing slowly or is born prematurely. No parent ever wants their baby to be taken away from them directly after birth and admitted into the NICU, but it's something that happens and happens fairly often. Abby and I never expected to have our baby girl in the NICU, but we found ourselves there on day 1. I work in hospitals for a living but spend most of my time in the OR, so when Hattie was taken to the NICU, it was a new experience for me. I knew about NICUs - the place where sick babies or babies born prematurely go - but spending a couple weeks there was a very unique experience. For me, the NICU had this vibe of resilience - a feeling of overcoming hardship and working towards a goal. Every baby had a goal, and the parents, doctors and nurses were focused solely on meeting that goal. I wanted to write a blog specifically about our NICU experience, what it was like, and how incredible the people who work in the NICU are. The NICU is a very special place, full of very special people.
NICU Part 1
Hattie was born kicking and screaming, and even bigger than we expected her to be. We knew she had microcephaly (small head) from the ultrasounds during pregnancy and knew she was growing a little slower than normal, but the pregnancy was never deemed "at risk" and we never expected spending time in the NICU. About 15 minutes after birth, they put Hattie under the warming lamps and swaddled her. I was looking at her with googly eyes, soaking in the fact that I was now a daddy. While Hattie had been kicking and screaming earlier, something didn't feel right while I was looking at her. She was calming down and her color was looking a little off. I notified the nurse who agreed and immediately unswaddled Hattie and starting patting her on the back. Hattie began crying and we really thought nothing of it. In "Hattie's Story", we explain what ended up happening... about four episodes of what everyone called 'dusky spells' where Hattie wasn't breathing properly and would turn a dusky gray color. We were in the NICU by that afternoon.
What we didn't know about hospitals with and without NICUs is that if you have a baby in a hospital without a NICU, they have to transport the baby to a separate hospital that does have a NICU via helicopter or ambulance. Because the mother is unable to be discharged until they are fully recovered, the father usually accompanies the baby to the separate hospital while the mother stays behind to recover. We were thankful to be in a hospital with a NICU, but have made a point to let future mothers know about this scenario. The more you know!
Abby and I stayed in the "Mom & Baby" area of the hospital where mothers would recover after giving birth. Every three hours throughout the days and nights, I would push Abby in a wheelchair down to the NICU to feed and hold Hattie. While it isn't necessarily a 'happy' memory in theory, I do look back fondly on those times - wheeling Abby down to the NICU at 3 in the morning to be with our new little girl. Abby and I really bonded during those days and nights - we really felt like a team and it was a defining moment in our marriage and beginning stages to parenthood. I learned everything in the NICU - how to change Hattie, how to feed her and burp her - and between my mom, Abby's mom and the incredible NICU nurses, I believe I received the best training possible!
Hattie was on oxygen immediately after being admitted to the NICU. They wanted to begin administering antibiotics, but were having a hard time finding a good access point with her tiny veins. I remember walking in to see Hattie, covered in needlestick marks - they had tried multiple times to get a needle in her arms, legs, feet and head. She had marks all over her. The doctors told us they would have to attempt a central line, meaning they would insert a tube through her belly button and into a main artery leading directly to her heart. It was a tedious procedure considering the danger of the tube entering her heart which could be fatal. They told us they were going to do this around 9p of our first night in the hospital. Abby was obviously worn out given the fact she had given birth that morning and gone through a stressful day. We got a phone call around 11p that the central line had successfully been administered and Hattie was receiving antibiotics. Breathing our first sigh of relief all day, we finally got some decent sleep.
Throughout that week, Hattie was doing great. Her blood cultures came back negative, her echocardiogram looked normal and she was acting like a normal, healthy baby. After 5 days in the NICU, we were home with our little girl. The night before Hattie was discharged, they let us sleep in a family room attached to the NICU. It was our first night together with all three of us... and Abby and I were scared, but considering I had been sleeping on a pull-out hospital futon for a week, I was pretty happy to sleep in a normal bed. Hattie did great that night - no tubes, cords or monitors. We were discharged that next morning and went home as parents to a beautiful baby girl.
NICU Part 2
We were back at the hospital after a couple days because Hattie's jaundice levels had risen. She was under the blue lamps that treat jaundice for a couple days, but fortunately it was a quick trip. We don't consider this another NICU stay, so the real NICU Part 2 was when Hattie had her episodes of respiratory failure.
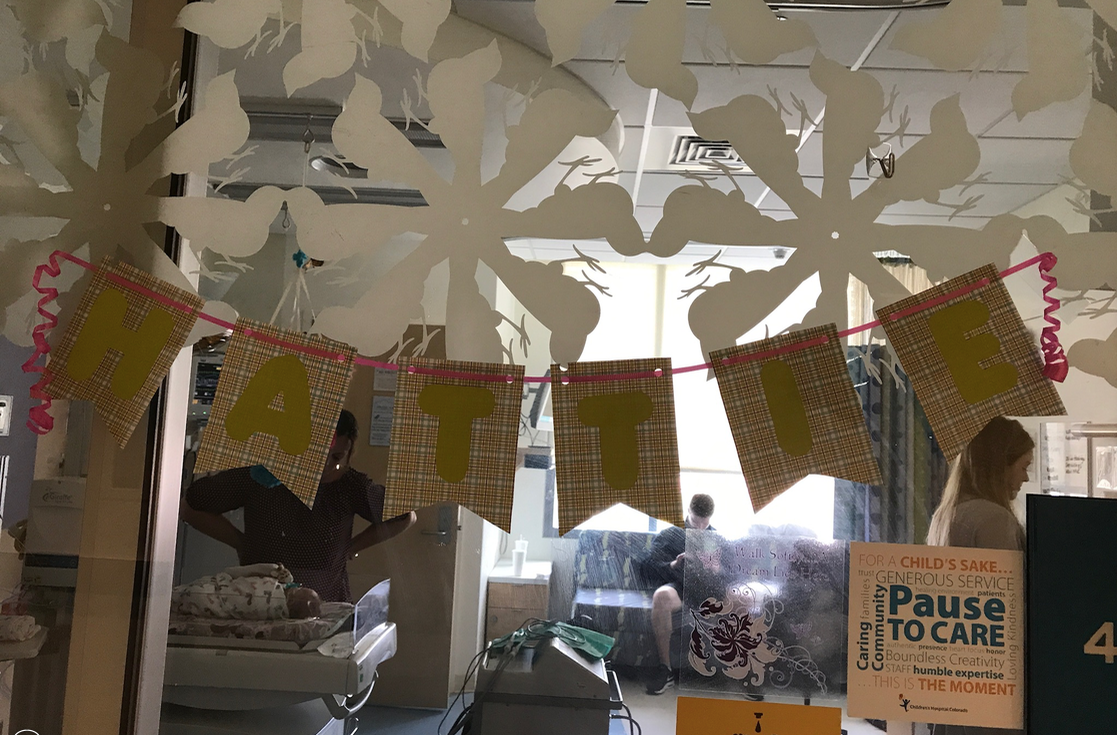
June 23rd, Hattie was taken in an ambulance to the emergency Room. Flight for Life transferred her to the large Children's Hospital in Aurora and we were once again in the NICU. It was a serious situation and we weren't sure how long our stay would be this time. The NICU Hattie was in directly after birth had about 20 or so rooms, but the Children's Hospital was a Level 4 NICU with 82 beds. We knew Hattie was in the best hands possible. She was immediately sedated and placed on oxygen and a feeding tube. We were assigned an attending neonatologist, a nurse practitioner and a nurse. Since it is a teaching hospital through the University of Colorado, we also saw many residents and fellows throughout the week. Our attending neonatologist was incredible - Dr. Mandell. Her attention to detail, knowledge and bedside manner is probably the main reason Abby and I made it through the week. She was and is an incredible doctor and an incredible person. There are days when Hattie is laughing and smiling and being sociable and I want to go back to the NICU and find Dr. Mandell and just say "Look what you did for Hattie! Look how well she's doing!" She was one of those people that we saw throughout the week that brought comfort and a sigh of relief in a very stressful and scary time. I don't know if she will ever read this or if we'll ever see her again, but Dr. Mandell was simply amazing. I don't know how else to put it.
Our nurse practitioner and nurses were equally as incredible. The hours they work in the environment they are in is rigorous, stressful and emotional. It's just different when there are babies involved. We got close to the staff that took care of Hattie and we think about them often. The Children's NICU was set up a little different as there was one nurse for every two babies. The nurse's desk overlooked the babies through glass windows, so every time an alarm went off, they had a view of the baby to observe and act accordingly. The nurses changed shifts every 12 hours at 7a and 7p and we started having the same nurses most days and nights. It was great to see a familiar face who knew Hattie's condition and progress.
Abby and I stayed in a family room connected to the NICU for the first two nights until we were 'evicted'. Parents of NICU babies will understand - your baby is hooked up to a monitor 24/7 tracking their oxygen saturation percentage, heart rate and respiration rate. This thing would start beeping randomly through the day and night and every time it went off, you immediately thought something was wrong. There were false positives a lot, sometimes her oxygen levels would drop when she was in deep sleep, and sometimes her heart rate would speed up - all leading to a blaring alarm that scares the absolute crap out of you. I still hear the alarm in my head sometimes. It got to the point where Abby and I knew in order to save our sanity and sleep, we would need to stay in a hotel. We met many parents who had been in the NICU for a long time. One family had twins who had been in the NICU for three months so far and had three months to go. When your baby is in the NICU for so long, staying in a hotel just isn't an option so the mom was commuting two hours a day from her home to the hospital to be with her babies. Many babies there were born prematurely, had surgery immediately after birth or were very sick.
Abby, her mom Tonya (Toa), my mom Sheri (Essie), and I got out one day for some much needed fresh air and a good lunch. The girls wanted to take some time to relax and get pedicures. I'm confident enough in my manhood to admit this was not my first pedicure, but it was a first time for one other thing. The girls all got their toenails painted pink for Hattie. Now, I wasn't about to miss out on supporting my baby girl, so obviously I also had to get my toenails painted pink. I'm not ashamed. As we left the nail salon, I put my shoes on and walked out the door, but not before a nail salon worker came running after me yelling that I needed some sealer or something to protect my new pink toenails from being damaged with shoes on. I have no idea how these things work. She made me sit on a bench outside so she could put some sealer over my toenails (picture below for your amusement).
Hattie had every test done under the sun her second time in the NICU - another echocardiogram, blood cultures, urine cultures, EEG (brain activity tracking), MRI, CT scan, daily reaction testing with the neuro team - and it got exhausting. Everything was once again looking normal until we received the results from her MRI. Her pons was smaller than normal and there were malformations in the ridges of her brain. This information led to the decision to send her blood panels off for genetic testing in Chicago. It would take about 6-8 weeks to receive results, but these results are what eventually led to us learning about her chromosomal deletion, 1q43-1q44. We finally felt like we had some answers. It was finally decided that the respiratory failure (and possible seizures) were due to the perfect storm of a urinary tract infection that had been detected and her brain malformations/chromosomal deletion syndrome. Looking back, we personally doubt she was having seizures as no seizures were ever detected on her EEG's throughout the week. Likely, her immune system was not built fully and could not handle the UTI, leading to respiratory failure. Either way, if she hadn't have had those episodes, we never would have found out about the chromosomal deletion. Dr. Mandell's persistence and determination to find an answer is what brought this information, and we are very grateful. We took Hattie home a little over a week later.
NICU Parents
We wrote earlier about how we felt a little guilty leaving the NICU, and it's true. There are many families that don't get to go home after a week. Parents who have had their kids in the NICU are some of the strongest people I've met. Having your baby whisked away right after birth is a horrible experience and having your baby in the hospital for six months is something I can't fathom. NICU babies themselves are little warriors. We would walk past the rooms of other babies, their names on the glass doors, and wonder what their stories were. I knew God gives special babies to special people, I just didn't know how special until I saw them first hand.
- David